Billie Rubin
RBCs: Taxi Cabs of the Cardio World
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Red blood cells are the taxi cabs of the cardio world. They can squeeze themselves into tiny capillaries or ride the big arterial highways like the aorta to different parts of the body. They are propelled by the currents created from the beats of the heart. They pick up oxygen molecule customers in the lungs and give it a ride to all the tissues of the body. The oxygen attaches itself to the iron at the center of the hemoglobin molecules (the taxi's red-velvet interior inside the RBC) and gets off where it's needed anywhere in the body.
The "empty" hemoglobin in the RBC then picks up another passenger in the tissues, a carbon dioxide molecule, and gives it a ride back to the lungs where the carbon dioxide gets off and is expelled through our breath. The “cab” works 24/7 for about three months until it’s worn out. It’s then removed from service and a new one takes its place. And that's life in the fast lane.
Buffy Coats
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
The term “buffy coat" might make you think of a shiny car wax, but in the world of blood banking, buffy coat refers to the white layer between red blood cells and plasma in a unit of whole blood after it has been spun down in a centrifuge. The buffy coat contains white blood cells, the soldiers of the immune system.

At SBC, we provide buffy coats for research purposes – primarily used to study immune response and other white blood cell functions. SBC’s founder and Medical Director, Dr. Ed Engleman, developed the methodology behind the first FDA approved cancer vaccine for advanced prostate cancer — a result of many years dedicated to studying these cells.
In addition, we can obtain fresh granulocytes, a specialized blood product comprised largely of white blood cells, from buffy coats. Granulocyte transfusions are given to patients with low white blood cell counts who have not been responsive to antibiotics. Click here to read about one little girl who received granulocyte infusions as a last-ditch effort to fight off infection resulting from her severe aplastic anemia.
Grateful in the Face of Challenge
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
It looks like our O+, O-, A+, and A- RBCs are going out to our hospitals at blinding speeds these days. When many of these blood types are at or near the critical levels in our inventory, everyone's work here at SBC is cut out for them. Finding and scheduling donors, setting up mobile blood drives, drawing the blood, testing it in the lab, and processing it for transfusion has our little hands working as fast as they can go.
We always have to stay ahead of the next emergency because when it happens, the blood has to be there. No matter what. But we feel grateful to be in a place with a wonderful infrastructure to face the challenge. From a community of volunteer donors, to state of the art technology for procuring, processing and testing blood, to a reliable and safe emphasis on the quality of our products. Think of how many countries do not have this, and be thankful that you are a part of this little miracle that happens every day.
Cytomegalovirus
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Cytomegalovirus (CMV) is a virus that 50 - 85% of adults have been exposed to at some point in their lives. It is passed by person-to-person contact with body fluids, and it is in the same family of viruses that cause chicken pox and mononucleosis. In healthy people, it rarely results in serious illness and can remain dormant in their bodies for the rest of their lives.
It can cause serious infection in babies, whether passed on through pregnancy or through a blood transfusion. Adults with weakened immune systems (cancer patients, transplant patients, HIV+ individuals) may also become severely infected. Because many cancer and transplant patients require the use of platelet products, we typically only provide hospitals with CMV-negative platelets. For this reason, testing negative for the virus is an important criterion for platelet donation eligibility.
A simple blood test will detect if a person has been infected with the virus. Stanford Blood Center was the first blood center in the world to routinely test for CMV and provide CMV-negative blood for immunocompromised patients.
For more information on our platelet program, please click here.
If you were a cell, which one would you be?
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
A heroic red blood cell - courageous, selfless, hard-working, picking up billions of oxygen molecules in the alveoli and coursing through the heart and every corner of the body electric feeding hungry tissues…
Or a quick bounding platelet - a cohesive force that brings everyone together to bond, hold hands across a gaping wound and save the waste of precious fluids and life itself…
Perhaps a mighty macrophage - a giant of a cell, a shape-shifter and relentless pursuer of evil, patrolling the body, taking care of its enemies and protecting all…
Or maybe a noble dendritic cell - the sentinel, the informer, the presenter of infectious evil to everyone in the immune world…
Perhaps you would be a stem cell - the creator, progenitor, mother, artistic source of all blood cells…
Which one would you be?
RBC Antigens - What Are They Good For?
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Red blood cell (RBC) antigens have to be good for something - nature doesn't make useless things for no reason. We have similar ABO antigens to some on bacteria, pollen, grains, etc., and these may be involved in stimulating the production of our natural anti-A and anti-B antigens.
RBCs have another antigen system as well called "Duffy" (abbreviated as Fy); one of about 29 systems of antigens like the ABO system. The most common antigens in the Duffy system are Fya and Fyb. Most people have one or both and it’s quite rare to lack both.
Well, it seems that some malaria sub-types (Plasmodium vivax and Plasmodium knowlesi, for example) can get inside RBCs via these Fy antigens (like a hand-hold). There is a large percentage of people in Africa or of African descent, however, that are of the rare type that lack Fy antigens. If you don't have Fy antigens, you stand a better chance against these types of malaria and your descendants have an evolutionary edge on survival. Very interesting...
Blood Group Linked to Gastric Bugs
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
It seems a rotavirus strain is using the sugar at the end of the type-A molecule as a doorway to the inside of cells. "A sugar molecule linked to type-A blood helps the rotavirus strain invade cells in the gastrointestinal tract,” a study has shown. “The virus is the leading cause of severe dehydration and diarrhea in infants, and causes an estimated 500,000 deaths worldwide each year. Specific blood group molecules are already known to promote infection by the stomach bug Helicobacter pylori (H. pylori) and norovirus."
Researchers found that an antibody targeting the type-A molecule blocked infection by the virus. "We never expected this," said study leader Dr. Venkataram Prasad, from Baylor College of Medicine in Houston, Texas. "Do other viruses use these blood group antigens as a door to enter the cell? The findings raise questions about why humans have different blood groups," said Professor Prasad, "One possibility may be that they evolved as a result of invasions by viruses or bugs." Type-A was the original "wild type". So, evolve into type-B and avoid rotavirus...makes sense.
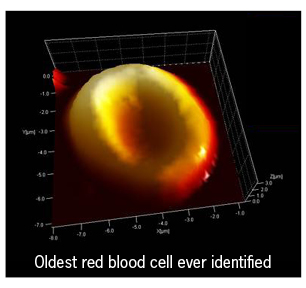
5,300 Year Old RBCs
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
In 1991, a couple hiking through the Italian Alps noticed something curious buried in the ice. What was assumed to have been the body of a fallen hiker, probably from a few years back, turned out to be “a 20th century archaeological sensation”. The remains were 5300 years old from a man who became known as Oetzi, a.k.a. The Iceman.
LiveScience reports that the Iceman “was so well preserved that scientists could estimate his age (about 45), his health and even his last meals (red deer meat with herb bread [but unfortunately for him, no Chianti]). His probable cause of death was thought to be an arrow wound to the shoulder that sliced an artery.”
Scientists studying Oetzi recently made an astonishing discovery. They were able to confirm that the donut-shaped structures found around the wound where the Iceman was fatally shot were red blood cells. The oldest human red blood cells ever to be studied.
Incidentally, his full genome was decoded a few months back. “It reveals that he had brown eyes, "O" blood type, and was predisposed to heart disease.” Oh, and he was lactose intolerant (5,300 years old with digestive problems, of course)...
Big Numbers in Our Blood
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Each of the approximately 30 trillion red blood cells (RBCs) in our bodies (30,000,000,000,000) has about 280 million hemoglobin (Hgb) molecules in it. And each hemoglobin molecule can transport four oxygen molecules from the lungs to any other cell in the body (including your brain, which is using that oxygen to read this right now).
So, what does this mean? It means that your blood is like a little tank of oxygen gas containing:
4 oxygen molecules x 280,000,000 Hgb molecules x 30,000,000,000,000 RBCs = a lot of molecules of oxygen that your tiny but mighty RBCs can carry!
Teenage RBCs
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Today is the first day of spring! Get ready to be wowed by flowers blooming, love blossoming, and newborn farm animals running around. Youth and spring make blood bankers think of reticulocytes, red blood cells that haven’t fully matured (the teenagers of the red cell world).
When these red blood cells (RBCs) are about ready to mature, they slip out of the bone marrow into the circulation to hang out in a corner and try to act like the big guys; and in about the space of one day, the young cells mature into adult RBCs.
Retics (as their friends call them) make up about 1% of RBCs and look a little different than mature RBCs. If their numbers in the blood circulation become higher than normal, it could mean that the RBCs are being destroyed, which makes the bone marrow crank out the young retics faster. So a reticulocyte count is an important piece in diagnosing certain diseases, such as hemolytic anemia. Ah, spring...
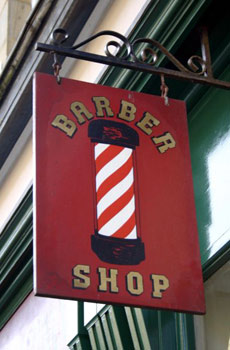
A Close Shave with Barber-Surgeons
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Phlebotomy was once a hair-raising occupation. The PBS series Red Gold: The Epic Story of Blood tells of a specialized medical practitioner that arose in the Middle Ages: the barber-surgeon. Not only could you get your hair cut at the barber shop, but the barbers performed some minor surgical procedures such as blood letting as well. They created their own guild, competed with doctors, and advertised their services with their unique barber's pole still in use today.
Their candy cane pole "represents the stick patients would grab while being phlebotomized; the white stripes represent the bandages and the red stripes, the blood." I wonder what medical history questions would have been like back then…
Incidentally, it was reported today on NPR’s Morning Edition that “Barbers in several states are pushing legislation to prevent shops without a licensed barber from using the striped pole. Some states are even proposing fines. They’re already in effect in Ohio and extend to pet grooming facilities, which can be fined up to $500 for using the pole.”
What’s next for Ohio barbers - phlebotomy?
What's in a Cell?
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Most living cells have a nucleus where the chromosomes and DNA live, and a number of other organelles that are involved in making energy, proteins, repairs to itself, etc. But our little red blood cell (RBC) friends selflessly throw all of that away when they grow up to have more room for lots of hemoglobin molecules that bind to oxygen, then take all that oxygen to other tissues of the body. This selfless act leaves our RBCs with a diminished life span (just 120 days) because they can't repair themselves.
RBCs are the most numerous of all cells in our bodies and they die at a rate of 2 to 3 million per second! But RBCs are produced as fast as they are removed. Our bodies recycle all the old parts that it can from a cell and send the rest out for compost or back out as CO2 that the plants can use.
Some Facts About Malaria
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
According to the Centers for Disease Control and Prevention (CDC), “About 1,500 cases of malaria are diagnosed in the United States each year. The vast majority of cases in the United States are in travelers and immigrants returning from countries where malaria transmission occurs, many from sub-Saharan Africa and South Asia.”
Malaria is caused by a parasite carried by mosquitoes that get it from an infected human. The parasite travels to the person's liver where it matures, then enters the bloodstream and infects the red blood cells (RBCs). They multiply inside the RBC, which breaks open within two or three days. The parasite then infects other RBCs resulting in the loss of hemoglobin, which can cause anemia, fevers and flu-like symptoms.
Malaria is treated as a medical emergency that requires a hospital stay. Chloroquine is often used for treatment, however, there is currently no vaccine.
Because malaria can be transmitted through blood transfusions, it’s important for us to ask blood donors about their travel history at each visit for screening purposes. Not sure if a location you traveled to within the past year is a risk area? Give us a call before dropping in: 888-723-7831. In addition, the CDC offers an interactive map application on their website.
How Did RBCs Evolve?
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Ill-conceived blood transfusions go back to the 1600's (disastrous transfusions of lamb's blood into humans), and the discovery of the ABO system goes back to the early 1900s. But just how old is blood itself? A picture from the Smithsonian in 2009 showed a red blood cell (RBC) in the soft tissue of a Tyrannosaurus Rex bone from 68 million years ago.
But blood cells go back, really far back. The first ones to evolve may have performed a mixed function of what white blood cells and red blood cells do now. Here's what the U.S. National Library of Medicine, National Institute of Health has to say: "The most primitive blood cell may have been a protohemocyte which was first involved in phagocytosis and nutrition. When metazoans (sponges) appeared [hundreds of millions of years ago], their "blood" cells, the archeocytes, were phagocytic. [Later] a progressive differentiation of several leukocytic types occurred. Differentiated cells appeared that distributed food and oxygen, thus erythrocytes evolved in certain marine or polychaete annelids [worms]."
In other words, the earliest ancestor of blood cells may have been one type of cell that provided both immunity and energy to the organism. Later, in what may have been sponges or marine worms, this “proto” blood cell evolved into several types of cells involved with immunity (WBCs) and other blood cells that distributed nutrients (plasma) and oxygen (RBCs).
Benefits of Blood Transfusions
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
A unit of blood does so much for patients in need. The gift of life is donated, tested, processed and sent to hospitals’ transfusion service departments where more important work is done to ensure it is compatible with the recipient.
Once the unit is ready to go, it has a number of advantages to offer. These are some of the benefits your donated blood can provide for patients in need:
1. Increase low hemoglobin levels: low hemoglobin can cause damage to body organs and tissues due to low oxygen levels.
2. Help stop bleeding: bleeding may not be controlled if platelets and/or clotting factors are low.
3. Keep the heart pumping: low blood volume can lead to low pressure and the heart may not be able maintain the circulation of blood.
4. Help with serious blood infections when other methods fail. Granulocyte transfusions, for example.
5. Provide red cells and platelets when the bone marrow is compromised: as with blood cancers, bone marrow transplants, chemotherapy.
6. Provide red cells and platelets for patients with blood disorders: such as sickle cell, thallasemias, myelodysplasia, aplastic anemia.
7. Save someone’s life.
Tiny Phlebotomists
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Historically, certain species of leeches have been used in medicine for blood-letting. These tiny phlebotomists were used in areas that were “too sensitive or confined for the lancet or other blood-letting instruments" like the gums, lips, fingers, and nose.
Leeches are sometimes in use even in modern medicine to ease venous congestion and prevent local coagulation in surgeries such as the reattachment of a finger or reconstructive surgery after cancer. According to the Journal of the National Cancer Institute, the leech “known as Hirudo medicinalis, the medicinal leech, is used most often after trauma, such as the loss of a finger or limb. Reattaching a digit and reconnecting its blood vessels is painstaking work that is often carried out under the microscope”. The leech has an anti-coagulant and anesthetic compounds in it’s saliva.
Leeches became popular in the 19th century to the point that they actually became endangered in Europe.
Incidentally, do you know how leeches got their name? According to medical secrets straight out of 1634, medieval doctors used to call themselves leeches. And it wasn't for their fees. The word "leech" comes from the Anglo-Saxon word "loece" which means "to heal". Interestingly, these creatures got their name from the doctors, rather the other way around.
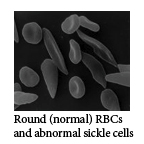
Sickle Cells
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Sickle cells are abnormally shaped red blood cells (RBCs) caused by a mutation of the hemoglobin gene (Hgb S). Their less flexible, sickle-like shape leaves them unable to get through small capillaries, resulting in obstructed blood vessels in many organs. In addition, because of this sickle shape, the RBCs are sequestered and destroyed in the spleen at a faster rate than normal cells.
It's been theorized that this abnormal sickle trait (i.e. one copy of the sickle gene) makes the RBCs more resistant to the malaria parasite, so this mutation may have provided an evolutionary advantage when inherited from only one parent. But when kids inherit Hgb S from both parents, it leads to a serious sickle cell disease and anemia. This can be a painful disorder and often requires many life-saving transfusions of normal RBCs.
Rarest ABO Type – Bombay Phenotype
| Tweet |
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Just in case the excitement of the ABO blood group system was beginning to subside, there is one other very, very rare ABO type first described in India. It is known as the "Bombay phenotype" and on the surface it looks like a type O. It is found in one out of 10,000 people in India, and one in a million in Europe.
The building blocks from which the A & B antigens are made is known as the H antigen. A and B genes transform most H's (not all) into As and/or Bs, respectively. Type O has the largest amount of "untransformed" H antigens.
Most people have HH or Hh genes but Bombay phenotypes don't. They are recessive hh. With no building blocks for A or B antigens, they look like a type O but they can make antibodies to the foreign H antigen - regular type Os don’t. They are incompatible with almost everybody! Only another Bombay phenotype can be transfused to them, usually from rare frozen inventories.
Shark Antibodies
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
It turns out that sharks are not just robust killers of the ocean but that they have robust immune systems, too. Who knew? They rarely fall prey to infections and are exceptionally resilient. According to studies at La Trobe University in Melbourne, their antibodies can attach themselves to human cancer cells and actually stop them from spreading. It may also be possible that their antibodies could be used to fight other conditions such as malaria or rheumatoid arthritis.
So if you ever come into contact with shark blood, perhaps you’ll be protected from certain diseases and conditions or from getting your wound infected. There's always a silver lining.
For more in depth information on this topic, visit La Trobe University’s website.
ABO Mutations
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
You may have heard of geometric shapes that are infinitely complex like clouds or snowflakes, but there's also our complicated little ABO (blood group) system. The four major blood types, A, B, O and AB, are controlled by just one gene on chromosome # 9 and the version of that gene that is inherited from your parents determines your blood type.
Easy enough. But deep down in the DNA, slight changes or mutations in that one gene can lead to even more versions (alleles). For example, about 45% of us are type A, but type A also has some rare subtypes like A2 and A3. About 100 of those mutations have been identified in the ABO system alone.
Then, in the Rh system, which determines the + or – following your blood type, 200 different mutations have been identified! And researchers aren’t sure they have found all of them yet. Fortunately, the testing the hospitals do can detect compatibility problems with very rare subtypes when they type the blood and test it with the patient’s blood before transfusing it.
Your White Blood Cells at Work
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Many of us are familiar with the role of red blood cells (RBCs) in taking oxygen throughout the body via the hemoglobin molecules they have inside, and of our platelets’ ability to help prevent bleeding through creating clots. But white blood cells (WBCs), our immune system warriors, are a little more mysterious. They make up a complicated system of T-killer cells, T helper cells, antigen-presenting cells, antibody-producing cells, plus others. When a unit of un-coagulated whole blood is spun down to separate components, the white blood cells appear, creating a thin, white layer between the plasma and RBCs.
There are five basic types of WBCs that are part of our immune system - neutrophis, eosinophis, basophils, lymphocytes, and monocytes. Of these, the first three are types of granulocyte WBCs; so called because they contain little granules filled with chemicals used to destroy foreign antigens such as bacteria or pollen.
Lymphocytes are special WBCs that make antibodies to bacteria and other foreign antigens. Monocytes are perhaps the most interesting of all the WBCs. They undergo a strange transformation as they squeeze through blood vessel walls into the surrounding tissues to attack foreign bacteria. The monocytes turn into macrophages (cells whose name means “big eater”) that can grow finger-like extensions called "filopedia". They reach for any bacteria with those fingers, bring them in closer, then eat them. They break them down with enzymes and eat their little bacteria bodies before the bacteria eat you.
Here is an electron microscope picture of one of these hungry macrophages and some E. coli bacteria.
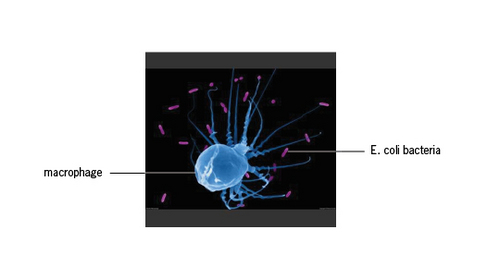
These are your WBCs at work. It’s a good thing they’re all there to protect you and keep you safe.
Magical Powers of the Color Red
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Red, the color of blood, was once thought to have magical powers. Cro-Magnon man painted the sick and dead red, hoping to contain the life force. Early Egyptians painted their bodies with blood to ward off sickness. Later, pastes and dyes were substituted in the practice - a forerunner of makeup. In early England, red coverings were put on beds to treat smallpox, and strips of red cloth were used as cures for scarlet fever.
In many indigenous Australian Aboriginal peoples' traditions, red ochre, a color-producing earth pigment, is considered “Maban” (a magical material), and is applied to the bodies of dancers for ritual. In some secret ceremonies, actual blood is used as it is believed to attune the dancers to the invisible energetic realm of the Dreamtime, the belief that an individual’s soul exist before their life begins and continues to exist after death.
What else comes to mind for you as an association with the color red?
Blood Collection in 1918
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Towards the end of WWI, blood collection equipment consisted of a 1,000cc glass bottle with two perforated rubber stoppers. Glass tubing through each stopper was attached to rubber tubing, each with a needle at the end. One needle was for the donor, the other for the patient (probably one soldier to another), and suction was created with a syringe.
The equipment was sterilized in an autoclave or boiled in distilled water, and the needles were sterilized just before use in boiling liquid petrolatum (petroleum jelly or paraffin).
About 500cc of blood was collected in a glucose-citrate solution. Then by reversing the same syringe that was used to collect the blood, a pressure pump was created to infuse it. No testing was required. You just gave the patient 15 to 20cc of blood, waited 15 minutes and if he didn't react negatively, you would transfuse the rest. Hearing this really makes us appreciate current testing procedures and blood banking standards!
Sugary or Sugar-free Blood: What’s Your Type?
By Billie Rubin
In an interview with National Public Radio (NPR), Dr. Christine Cserti-Gazdewich, a hematologist at the University of Toronto, educates us on the history of blood types.
"Blood type is a fascinating thing. Most anciently humans, or pre-humans… began as group A. A is the most ancient, so-called wild type. That's what we call genes - the way they start before they begin to mutate and turn into things that exhibit selective survival advantages. So about five million years ago, this mutation pops up called group O. And around that time, and subsequently, group B developed. Group O is actually a non-expression mutation. So A, B and O relate to what kinds of sugars you decorate your cells and secrete into your plasma and other secretions. Your A sugar is something with a messy name called GalNAc or N-Acetylgalactosamine. B is galactose. And it turns out that group O is actually a non-sugar or sugar-free status cell.” You could say it's the Splenda of blood!
Click here to be taken to NPR’s website where you can listen to the complete interview.
A Magic Potion
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Cryoprecipitate is a blood product made from frozen plasma. The plasma is slowly thawed, then sent through a centrifuge, a machine that spins and sorts blood components based on their masses. The “cold precipitate” protein that is left behind after most of the liquid plasma is removed is the cryoprecipitate.
Cryoprecipitate, or “cryo” as it is affectionately called, originally found use as treatment for hemophilia. It was discovered that cryo had concentrated quantities of Factor VIII, a blood-clotting factor. These concentrates are transfused in pools of five or six. (Coincidentally, this discovery is in part due to Dr. Judith Pool, a Stanford researcher and professor in the 1960s and 70s.)
Before cryo, hemophiliacs had to be transfused with frozen plasma to help control their bleeding. However, all of the extra fluid in the frozen plasma could lead to circulatory overload and congestive heart failure. So, this magic potion revolutionized the treatment of hemophiliacs!
The Life of a Red Blood Cell
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Red blood cells (RBCs) are born in the bone marrow of our large bones at a rate of 2 million every second! Our bone marrow is like a heavy-duty erythropoietic ward.
And RBCs grow up fast. In about seven days they are ready to toss out their nucleus and DNA and leave the nest to spend all of their 120-day life span traveling down vast arterial highways and capillary byways. They get rid of their interior baggage so they can each carry over 250 million molecules of hemoglobin. While tossing out their DNA makes them beefier, it also limits them as they can't reproduce or even repair themselves. It's a wild life.
Erythropoietin & Your Red Blood Cells
By Billie Rubin
Guess who regulates how many red blood cells (RBCs) we need at any given time. Bone marrow? Liver? Spleen? Your lungs? Give up? It's your kidneys. Yup, they don't just make urine. It all starts when those little kidneys sense the level of oxygen in our blood. When the oxygen level is low, the kidneys put out a hormone called erythropoietin.
The bone marrow has special receptors for the erythropoietin and when it gets some, it starts to crank out RBCs. As more RBCs mature and start picking up oxygen in the blood and taking it to various tissues, the kidney senses that the oxygen level is now okay and stops producing erythropoietin and the bone marrow slows down for the time being. Interesting feedback loop, eh?
Apheresis: It's Greek to Me
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
In Greek, apheresis means "to remove or to separate a part from the whole.”
Here are a few facts from the "Core Curriculum for Nephrology Nursing”:
• In the 1940s – Dr. Edwin Cohn adapted a cream separator machine to separate plasma from whole blood for use in injured soldiers during WWII (and to prepare half & half for tea).
• In 1951 – Human plasma was made commercially available.
• In the 1950s – Dr. Cohn, while at the Harvard Medical School, invented the “Cohn Fractionator”, which was successful in separating blood into all of its components.
• In 1987 – COBE Spectra introduced a continuous-flow centrifugation device used for plasma exchange, cytapheresis and other clinical applications.
Thus the dawn of apheresis began and we can now separate the various parts of your blood, allowing us to collect only the specific components needed for patients that day. It's a very efficient way of directly helping patients in hospitals!
To inquire about apheresis donations, please call 888-723-7831.
How Are Blood Component Expiration Dates Determined?
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
The Food and Drug Administration (FDA) and the American Association of Blood Banks (AABB) set safety standards and requirements that blood banks must follow. One of these is the expiration date of various blood components. For red blood cells, the date depends on the types of anticoagulants and additive solutions; the most common systems currently in use have an expiration date of 42 days from the date of collection. But if the hermetic seal at the top of the blood collection bag is opened (when preparing to transfuse a unit), the expiration date is just 24 hours.
The FDA requires that the expiration date be exactly one year from the date of collection for frozen plasma. Platelets expire five days from the date of collection because they cannot be refrigerated.
The FDA sets these dates on the basis of safety and viability studies.
Type B: Passionate, Excitable, Creative Types
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Type B+ blood is found in about 8.5% of people in our population, and B- is found in only 1.5%. Type B red blood cells have the B antigen on their surface and anti-A in their plasma. There's a popular belief in Japan that ABO blood types, in a manner similar to western astrology, can predict personality and compatibility. Type B individuals are said to be passionate, creative and excitable. Type A folks on the other hand are thought to be conservative, introverted and calm. Ring true?
Iron (Fe) & the 56-day Deferral
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
The 56-day interval between whole blood donations is not just to build up our red blood cell (RBC) and hemoglobin levels again but also to give the body enough time to collect the amount of iron it lost in the donation. Our bodies can make their own hemoglobin and RBCs in the bone marrow and liver and do so constantly, but it can't make iron.
We get iron from the foods we eat or in supplements. And it's the iron at the center of the hemoglobin molecules that binds to oxygen (and carbon dioxide). That's how RBCs transport these gases throughout the body.
The Perfection of Red Blood Cells
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Red Blood Cells (RBCs) have some particularly unusual characteristics for a cell. For one, they have a biconcave shape, giving both sides a "scooped-in" appearance.
They also lack a nucleus when fully mature. These traits help them do the job they do. Without a nucleus they have more space to carry the gases they transport (oxygen and carbon dioxide). They also have less mass. If RBCs had a nucleus, blood would have more mass and the heart would have to work 20% harder.
In addition, the RBC's biconcave shape gives them more flexibility to squeeze into small capillaries (which are only slightly larger than the RBC itself) and a maximum surface area to facilitate the transfer of the gases they carry. They are the picture of perfection for just what they do.
The Four Humours
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Once upon a time (from early Greek and Roman physicians to the late 19th century), "blood-letting," now known as phlebotomy, was a very popular practice to cure or prevent illness. The theory was that a mystical equilibrium between several bodily fluids (humours) maintained human life. Excess blood would disturb that balance and result in illness.
The four humours were: black bile, yellow bile, phlegm and blood. Too much black bile made you melancholic, too much yellow bile made you choleric, too much phlegm made you phlegmatic, and too much blood made you sanguine. The four humours were related to the four elements: earth, fire, water and air. All four of these elements were said to be in the blood in the form of humours.
So, next time you see those blood bank phlebotomists out there, remember they are not just collecting blood, they are practicing the most ancient form of healing: bringing equilibrium back to the people.
Where Are the A & B Antigens on a Red Blood Cell?
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Well, think of a little red blood cell (RBC) in 3D with lots of tiny little hairs sticking out of it. Type A people have about 1,000,000 of these hairs on each RBC and at the end of the hair is an A. Type B people have about 700,000 hairs with a B at the end of it. And AB people have about 600,000 hairs with A's and 700,000 hairs with B's at the ends. Don't you wonder who in the world counted these hairs? Science is strange.
Then of course we have the type O's. They just have lots of hairs with nothing at the end of them. The hairs are so tiny that you can't see them under a microscope, but they are lurking there, believe you me...They are little chemical structures on the RBC membrane that determine the ABO type (along with the antibodies in your plasma).
Really Big Hearts
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
When your heart is all aflutter, who do you resemble most? Romeo & Juliet? Lady Chatterley? Anais Nin and half of Paris? Or possibly a hummingbird if you are really feeling verklempt.
While our heart rate may go up to slightly more than 100 beats per minute when in the presence of our beloved, a hummingbird's resting heart rate is 615 beats per minute! Their athletic fluttering uses up quite a bit of energy and they need the extra oxygen that their big hearts pump out. Their hearts are about 2.5% of their body weight, whereas ours is just 0.45%. They have the really big hearts of the world with some major blood circulation going on. Imagine blood collection from them... they would need a very, very small needle (butterfly needle, perhaps?) and taking their pulse would be a marathon!
Happy (early) Valentine’s Day ☺
Why Am I This Type?
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
This is one of several questions that we’re often asked by community members. Our ABO (blood type) identity, whether we're O, A, B, or AB, is inherited from our parents. The ABO genes we inherit produce the antigens (chemical structures like proteins, carbohydrates or glycolipids) that are attached to the surface of red cells. Other things in nature also have these A & B antigens (bacteria and pollen, for example).
After birth, when our bodies are exposed to a foreign antigen (one you did not inherit), our immune system makes antibodies against it. If you are type A, then B is foreign to you and you make anti-B. If you are type O, then both A & B are foreign to you and you make anti-A and anti-B. These antibodies float around in the plasma portion of the blood. Both the ABO antigens on the red blood cells and the anti-A and/or anti-B in your plasma, determine your ABO Identity. Being Rh + or - is inherited separately from our ABO genes and it's a little different. Read more about that here.
Groundhog Sees Shadow of His A & B Antibodies
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
What does that mean?? Is there a blizzard coming? Cyclone? Mongoose? Groundhogs don't even see very well so who knows why we rely on them to tell us about when Spring is coming. Best to look for when inexpensive daffodils show up at Trader Joe's, or when your allergies start up again. Then you know pollen is in the air, and with pollen comes an increase in your anti-A and anti-B titers. Wonder why? It's because our red blood cells (RBCs) are not the only things sporting A & B-like antigens on their surfaces. Other environmental antigens, similar enough to those little sugary ends of our RBCs, can show up in bacteria, pollen, and viruses and stimulate an immune response in us (plus other allergens). The groundhog knows the power of his antibodies and comes out every February 2nd to check them out to make sure not many foreign antigens get past his immune system this Spring.
Mooootations

By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Here's something interesting about blood types. Humans have 8 major blood types (although we also have hundreds of lesser-known mutations or alleles that are very rare). We collect and transfuse O+, O-, A+, A-, B+, B -, AB+ and AB- red blood cells, platelets and plasma.
But did you know that cats have at least three major blood types, dogs have at least four, and cows have 800 different blood types? It's no wonder some of those cows are mad…it must be hard to get some compatible blood in that pasture. What a collection nightmare...100 times the current work of finding enough of those 800 blood types to meet our Jersey friend’s needs. So, there you have it, there's always a silver lining.
Our Inner Ocean
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Did you ever wonder what plasma and sea water have in common? Considering it's our "inner ocean" and that life may have originated in the sea, they are very similar. The only differences are in the salinity (more in sea water = a higher osmotic pressure) and plasma has some proteins and organic compounds not found in sea water.
Our plasma is 90 - 92% water (much fresher water than the ocean) and the other 8 - 10% is the materials it transports to and from all cells (fibrinogen, sugars, hormones, amino acids, cholesterol, lipids, urea & other waste products).
More than half of our blood is plasma and the rest (35 - 40%) is red blood cells, white blood cells, and platelets. So what does all of this mean?? It means that 50% of the time we are donating, collecting, processing and distributing... water! Just like Alhambra or Evian. Well, maybe more like vitamin water (with urea & organic stuff in it).
Type A Cats
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Cat blood is designated as either type A, type B, and rarely type AB. Type A is the most common blood type comprising 90-95% of the cat population in the United States. While type B cats are uncommon, it is extremely important that they be given type B blood. Less than 1 ml of blood from a type A cat that is given to a type B cat can cause a transfusion reaction strong enough to result in death (because of the Anti-B that type A cats have in their plasma).
Cats that are type AB can receive blood from either type A or type B cats (that’s cats, not us). Cat blood is screened for a number of blood-borne infectious diseases as well as feline leukemia and FIV. If we continue with our type A shortage, we may look at our cats in a whole new way...
How Long Do Red Blood Cells Live?
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
A unit of red blood cells (RBCs) expires in 35 or 42 days because of the type of anticoagulant in the bag. But in real life RBCs live about 120 days (except for Scarlett O’Negative, she’s immortal). When they get old and their membrane starts to show wear and tear (like most of us), they get removed from the blood circulation in the spleen, liver and bone marrow at about the same rate as new ones get produced. It's the original "sustainable" environment.
There are millions of RBCs in just one drop of blood. People who live at higher altitudes have more (like in the mountains of Peru). They are produced in the bone marrow of large bones at a rate of 2 million per second. In the minute it took you to read this, you made 120 million of them!
What Do Monkeys & Rabbits Have To Do With it?
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Most of our blood donors probably already know that the positive or negative after their blood type (A+, B-, for example) represents their Rh factor, an antigen present on the red blood cells of some people. Persons with the factor are designated Rh-positive, those lacking the factor are designated Rh-negative.
Being Rh-positive or Rh-negative really means that either you have the D antigen on your red blood cells or you don't. Rh(D) is inherited separately from our ABO genes. If you inherit a dominant Rh(D) from one or both of your parents, you are Rh-positive. If you inherit the recessive rh/rh genes from both parents, you are Rh-negative, which represents just 15% the population.
Now here’s something you may not know. It seems we have rabbits and monkeys to thank for the discovery of the Rh system. In the early part of the 1900's, Karl Landsteiner, who discovered the ABO blood typing system, and Alexander Weiner, an important Rh system researcher, injected some rabbits with blood from rhesus monkeys. The rabbits naturally objected and produced antibodies against the monkey blood. Then an interesting thing happened. That same rabbit antibody against the monkey blood also reacted with some human red blood cells. That's right, with Rh-positive people, 85% of us to be exact. Don't you wonder where those two docs got the idea of mixing monkey blood with rabbits?
Red Blood Cells & Stardust
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Made for Each Other
What does the center of the earth have in common with the center of our Red Blood Cells (RBCs)?? Fe: Iron. The center of the earth is a molten mass of iron and it just so happens that iron is also at the center of all of our hemoglobin molecules. Interesting, no?
In our hemoglobin, iron holds on to oxygen as the RBCs pick it up from our lungs and deliver it to the tissues that need it all over our bodies. Our bodies can't make iron. We get it from food and our food gets it from the earth. This is the reason why we must wait 56 days between blood donations, so we can replace the iron stores in our bodies. It's quite the circle of life.
By the way, the earth got its iron from the stars. So our RBCs are most definitely made from stardust, right?
The Japanese Blood Drop
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Meet Kenketsu-chan ("blood donation girl"), Japan’s most well-known blood donation mascot. She is a little pixie with big shiny drops of blood for ears. Kenketsu-chan is the official blood donation mascot of the Ministry of Health, Labour and Welfare, which maintains a website devoted to the character. It is said that Kenketsu-chan’s ears shrink when she runs low on blood, but return to their original size when people donate (see the different images above). She comes from Tasuke Island (Help Island), which features a heart-shaped spring at its center. The spring shoots forth rainbows that carry Kenketsu-chan to wherever people need blood.
Hmmm, what should we use for our official mascot?? Any ideas?
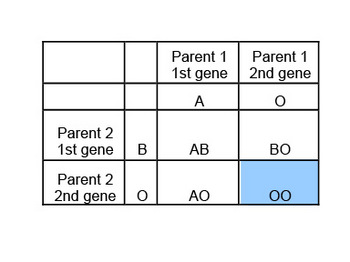
ABO Dominant and Recessive Genes
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Here's an interesting trivia question: Can a man who is type A and a woman who is type B have a type O baby?
a) Only if the baby is adopted
b) Only if the blood was mistyped
c) Yes
The answer is yes! They have a 25% chance of having a type O baby. We actually have two ABO genes, not one. We inherit one ABO gene from dad and one from mom. In this case, one parent would be AO and the other BO. And each could pass either gene to the baby. You just don't know they are AO or BO until you do family studies because the O gene is recessive (the blond, blue eyes of the ABO world), and an AO person looks like an A when you type them and a BO person looks like a type B. A type O person would need two recessive genes (OO). Here’s a chart that explains the four possible ABO types of the children:
Blue Blooded Relations
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
The next time you hear somebody say they have "blue blood" in their ancestry & are trying to tell you that they are of royal blood lineage…think "molluscs." Because they must have a high class horse-shoe crab, clam, squid, or octopi in their family tree.
Molluscs are the true blue bloods of the world. Their blood is truly blue when they bleed because instead of hemoglobin, they have a copper-containing protein called hemocyanin which turns dark blue when exposed to oxygen. So, try to be understanding of your blue-blooded friend: their great, great grand-daddy was a royal horse-shoe crab, and they are proud of it.
The Spirits in Blood
By Billie Rubin, Hemoglobin’s Catabolic Cousin, reporting from the labs of Stanford Blood Center
Back in 1668 when there were a few experiments of blood transfusions from sheep into humans, the reason for doing this wasn't that sheep were plentiful or made good blood donors (no malaria travel), but they thought that the blood from a gentle creature might quiet the "tempestuous spirit of an agitated person." You probably know one of those people that could use some sheep blood…
It was also thought that the shy might be made more outgoing by the blood of more sociable creatures...dogs probably, high spirited ones like Chihuahuas and Golden Retrievers. Their donor history questions might have gone something like this: "When was the last time you bit anyone?" "Do you have a history of rabies or heart worms?" "Have you received any vaccinations against parvo?" "Do you feel well today, any kennel cough?" Woof!