Centers
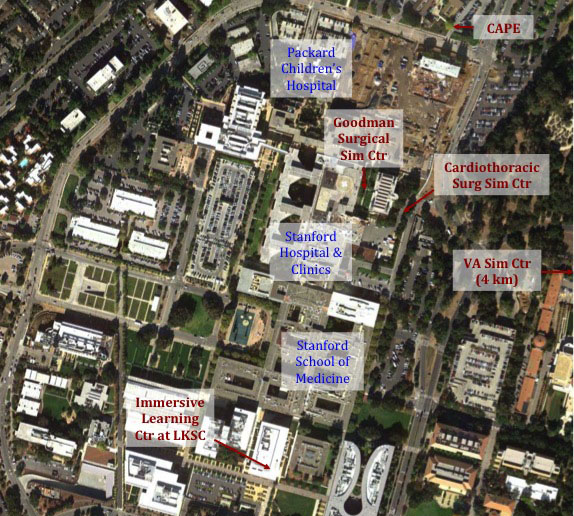
CISL has several core simulation groups and a number of simulation facilities. These include (in order of establishment):
The Immersive Learning Center (ILC) in the Li Ka Shing Center for Learning and Knowledge
The practice and science of medicine cannot be learned solely via passive means. Caring for real human beings is an active process; preparing students, interns and residents, and experienced physicians and teams for the rigors of medical practice requires facilities and programs of active learning. Stanford is a world pioneer of various forms of Immersive and Simulation-based Learning, which represents the most intensive forms of active learning in medicine. With the goal of revolutionizing the education and training of all our learner populations. The Immersive Learning Center – occupying the entire ground floor of the Li Ka Shing Center for Learning and Knowledge – brings together all modalities of simulation and novel forms of immersion into one place for the first time. The Immersive Learning Center will allow medical students and others to integrate their classroom understanding in parallel with simulation-based practice. Creating a virtual microcosm of a clinic or hospital in the ILC, learners can seamlessly maneuver through a variety of complex medical settings without worrying about making mistakes.
Below is a list of the various offerings in the ILC.
• Project Classroom – this space gives students an opportunity to practice “messy” practical procedures like placing plaster casts.
• Simulation Suites -Four large simulation rooms and 10 clinic rooms flexibly replicate different clinical settings, including an operating room; a multi-bay emergency department or intensive care unit; single-patient hospital rooms or critical care isolation rooms.
• Task Training Space –Part-task trainers and other simulators will be available for teaching specific medical procedures or surgical operations.
• Virtual Worlds – A unique site in the ILC houses a dedicated room to enable the use of role-playing healthcare “virtual worlds” (similar to online multiplayer games such as “World of Warcraft”™) to allow student-controlled avatars to represent nurses or doctors in a trauma ward and respond to a patient’s changing condition.
• Immersive Interactive Room – This space with a raised floor and intensive information infrastructure will support high resolution imaging displays, HD-quality telepresence video-conferencing, and eventually “mixed-reality” virtual reality simulation.
Patient Simulation Center of Innovation
at VA Palo Alto Health Care System
The Simulation Group at VA Palo Alto is the pioneering inventor of modern mannequin-based patient simulation. They performed their first pilot-test simulations in 1986, and have had a dedicated simulation center since 1995. Besides inventing the modern simulator technology they are responsible for introducing the current paradigm of high fidelity simulations addressing both behavioral and teamwork skills as well as technical/medical skills, adapting many concepts and practices from those used in commercial aviation simulations.
Originally concentrating on anesthesiology – the field of pioneers Gaba, Howard, Fish (and now including Drs. Harrison, Fanning, and Mudumbai), the Group has expanded to include Stanford faculty working on simulation in Intensive Care and Rapid Response Teams (Lighthall, Barr, Geller, Bertaccini), Emergency Medicine (Harter and Smith-Coggins), Respiratory Therapy (Miller and VA Palo Alto RT staff). A spin-off group in pediatric anesthesia (Chen, Edler, Honkanen, Williams, Hackel) conducts simulation training in actual clinical work environments. This group also conducts research on performance assessment and on testing of human factors of medical devices and procedures using simulation.
This Group a long-standing dedicated simulation center. Currently occupying around 2200 square the VA Simulation Center has 2 large simulation rooms – one set up as on operating room and one as an ICU, ED, or Ward. This Center has 5 simulators – 3 permanently set-up and 1 adult simulator for “in-situ” training exercises in actual clinical environments. The VA group provides the infant simulator to the pediatric anesthesia simulation team.
Center for Advanced Pediatric and Perinatal Education (CAPE)
Work on neonatal and pediatric simulation began in the late 1990s by Lou Halamek, MD at the VA Simulation Center (veterans have children and grandchildren too!). Philanthropy enabled the group to create the CAPE facility near the Lucille Packard Children’s Hospital at Stanford.

CAPE develops, conducts, and evaluates training in neonatalogy, perinatalogy (including combined-team training linking obstetrics, OB anesthesia, OB nursing, neonatal intensive care, and neonatal transport. CAPE has one large simulation room with two simulation bays and several different simulators (maternal and neonatal). CAPE also conducts research on simulation pedagogy and on human factors.
The Goodman Simulation Center
The Goodman Simulation Center, under the direction of James Lau, MD is located in close proximity to the operating room suites at Stanford Hospital. This center will utilize mannequin based team training, and a training program for laparoscopic surgery using part-task trainers. The ultimate goal is surgeons will rehearse an operation on a patient-specific palpable hologram that is digitally derived from models that are constructed from diagnostic imaging data and later, deliver the data set of that operation with robotic assistance.
The surgical curriculum, from PGY1 to PGY5 will incorporate simulation-based training to build the skills of the novice practitioner to fine-tuning the skills of the advanced resident preparing for practice.
Endovascular Simulation Program – house in the Goodman Surgical Simulation Center under the direction of Jason T. Lee, MD. Beyond the Division of Vascular Surgery, the endovascular simulation program offers housestaff training and continuing medical education programs in cardiology and interventional radiology.
Cardiothoracic Surgery Simulation (CVS-Sim Center)
Located within the Falk Cardiovascular Research Center, the CVS-Sim Center contains thoracic models, arrested heart models, model for beating heart surgery, anastomosis and valve replacement task stations, intra-aortic balloon pump station, perfusion equipment, cardiovascular surgical instruments and supplies, operating table, video recording capability, porcine hearts for wet-lab, computer with educational DVD/CDs, and reference books and other educational materials. Based on a series of task/skill stations, wet-lab procedures, and environmental simulation, we have developed a comprehensive program intended to provide initial and follow-up simulation training and practice of cardiovascular surgery for the surgical resident.
The laboratory along with the CVS simulation course provides an environment for cardiac surgery and general surgery residents to practice cardiac surgical techniques and procedures. The simulation laboratory is designed to permit the resident to engage in a progressive experience; each task or sub-procedure is intended to allow the resident to demonstrate proficiency through direct tutoring and practice in the laboratory and in the simulated operating room. Directed by Drs. James I. Fann and Thomas A. Burdon, the CVS-Sim Center is a part of the Stanford Cardiothoracic Surgery curriculum.