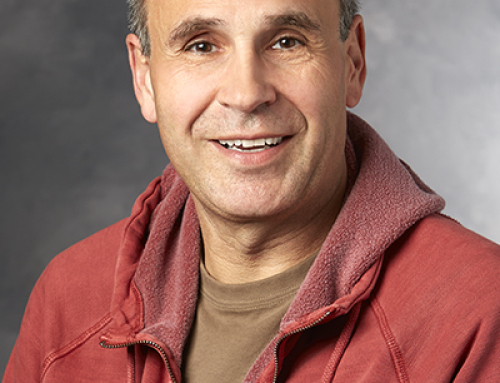
Dr. John Oghalai treats adults and children with hearing loss at the Stanford Hospital and Clinics and the Lucile Packard Hospital Children’s Hearing Center at Stanford. He is a clinician-scientist with the goals of better understanding the fundamental changes in the inner ear that underlie progressive hearing loss and to develop novel techniques to treat this problem before it leads to deafness. Ultimately, he strives to improve human health not only by expertly caring for his patients, but also by advancing scientific knowledge so that all physicians can treat hearing loss more effectively.
Dr. John Oghalai treats adults and children with hearing loss at the Stanford Hospital and Clinics and the Lucile Packard Hospital Children’s Hearing Center at Stanford. He is a clinician-scientist with the goals of better understanding the fundamental changes in the inner ear that underlie progressive hearing loss and to develop novel techniques to treat this problem before it leads to deafness. Ultimately, he strives to improve human health not only by expertly caring for his patients, but also by advancing scientific knowledge so that all physicians can treat hearing loss more effectively.
Dr. Oghalai grew up in Madison, WI and received his undergraduate degree in electrical engineering and degree from the University of Wisconsin, Madison. He then moved to Houston, Texas in 1994 for residency training in otolaryngology – head and neck surgery at Baylor College of Medicine, during which period, he spent two additional years in the basic science research lab studying hair cell physiology.
Dr. Oghalai carried out additional training in otology, neurotology and skull based surgery at the University of California, San Francisco, prior to returning to Baylor College of Medicine as an Assistant Professor and later Associate Professor.
In 2010, Dr. Oghalai joined the Department of Otolaryngology Head and Neck Surgery at Stanford University School of Medicine and became the Director of the Lucile Packard Children’s Hearing Center at Stanford. He is currently a member of both the Division of Otology & Neurotology and the Division of Pediatrics Otolaryngology.
“Hearing Loss is a symptom – not a diagnosis.” – Dr. Oghalai
A key area of Dr. Oghalai’s research is the imaging of the inner ear. This is an area of great importance as currently when a patient is determined to have hearing loss, physicians may be able to identify a cause, such as genetic mutation, or environmental exposure. However, due to a lack of ability to image the inner ear, they are most likely unable to tell the patient exactly what has occurred within their own inner ear, such as loss of hair cells in a particular region of the cochlea.
Because of the current difficulty in performing auditory research in humans, Dr. Oghalai’s lab studies normal and transgenic mice that have hearing loss. They strive to perform comprehensive evaluation of the pathophysiology that creates the hearing loss. For example, cochlear function is monitored with measurements of the compound action potential, the auditory evoked brainstem response, distortion product otoacoustic emissions, the cochlear microphonic, and the olivocochlear reflex. Basilar membrane motion is measured using laser doppler vibrometry. Histological study of the inner ear is performed using immunohistochemistry. They also use the patch-clamp technique to study hair cell physiology. Recently, they have begun using fluorescent-activated cell sorting (FACS) to isolate outer hair cells from the adult cochlea after noise or blast exposure to study the regulation of genes after cellular injury.
Excitingly, they are also working on techniques to be able to perform research in humans. The Oghalai lab is in the process of developing novel optical techniques for in vivo imaging using Optical Coherence Tomography (OCT). The level of detail within the cochlea that they can now image is roughly two orders of magnitude better than what is currently available with the latest MRI or CT techniques. Their goal is to be able to identify why any given patient who comes to clinic has hearing loss, and use this information to guide management using regenerative strategies that are in active development.
Most recently, Dr. Oghalai and colleagues reported findings in the publication PLOS One on Blast Induced Hearing Loss. This paper reported the exciting findings that hearing loss from loud blasts, such as roadside bombs or other explosions, might not be irreversible, as previously thought. Hearing loss and tinnitus are the most common service related disabilities, and the use of explosive devices (IEDs) is on the rise worldwide. These findings give hope of the development of future treatments which could make a large difference in the lives of military personnel, veterans and private citizens who have sustained a blast injury.
In the clinical setting, research is focused on improving what is currently done to help children with deafness. Cochlear implants (CI) are the most common treatment for deafness. While many factors influence the ability of a deaf child who is hearing through a CI to develop speech and language skills, an important factor is to properly program the CI. However, implementing the optimal CI program is a challenging, individualized, and iterative process with variable success. Therefore, the Oghalai lab is developing the technique of near-infrared spectroscopy (NIRS) to functionally image activity within the auditory cortex of children hearing through a cochlear implant.
Dr. Oghalai is also running a multi-site, prospective randomized clinical trial of deaf children with special needs. The goal of the study is to determine the best treatment options for children who require such complex and individualized care. This trial is actively enrolling participants at Lucile Packard Children’s Hospital in Palo Alto, CA and at Texas Children’s Hospital in Houston, TX.
Please join us in congratulating Dr. Oghalai on his recent paper on Blast Induced Hearing Loss and his continuing excellent work on advancing the understanding of hearing loss and towards its eventual cure.
If you would like to support Dr. Oghalai’s research, please consider making a generous donation.