Behind method for activating adult stem cells, a shaggy-mouse story
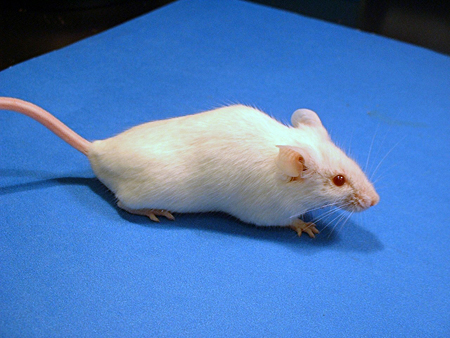
Out of the tousled tresses of a long-locked mouse, Stanford researchers have discovered a technique to turn on certain adult stem cells at will. Their new method not only transforms shorthaired mice into shaggy critters but also could open the door to finding ways to use stem cells to treat a host of tissue-related diseases and conditions, including cancer.
"Any area that requires tissue regeneration could be potentially impacted by this finding," Dr. Steven Artandi, an assistant professor of medicine (hematology), said of the research, which was published in the Aug. 18 issue of the journal Nature. Artandi is the senior author of the paper that focuses on stem cells in the mice's skin tissue, though it has implications for other stem cells as well.
The key to controlling these stem cells lies within an enzyme, telomerase, which has long been known to play a crucial role in keeping chromosomes intact when stem cells divide and in the formation of cancer. There is recent evidence, though, that the enzyme may play additional roles in the cell that are not well understood.
To better understand the role of telomerase, Artandi's lab developed a genetically modified mouse, which enabled them to stuff additional telomerase into the mouse's cells. The added enzyme was equipped with a genetic switch that would activate telomerase, or more specifically a telomerase component called TERT, when the mouse was fed a chemical trigger.
Similar to the board game Mouse Trap, in which one trigger sets off a chain of events ending in the capture of a mouse, the chemical trigger fired up the TERT, which kicked the stem cells into action, which built up the hair follicles, which started growing hair nonstop, which ultimately yielded the shaggy mouse.
Adult stem cells in hair follicles are only intermittently active, so hair normally grows in corresponding spurts. When active, the stem cells proliferate and expand, building up the follicle and producing cells that make new hair. After a while, the follicle reverts to a resting state and hair growth ceases. But all that changed when Artandi and Kavita Sarin, lead author of the paper and a Stanford graduate student in genetics, flipped the switch on the TERT gene. The stem cells woke up and stayed up.
The finding is particularly striking because the TERT protein was acting independently from its normal role in the telomerase complex. "TERT can activate stem cells and cause them to proliferate," Artandi said. The introduced TERT was present in other tissues besides the mouse's skin, where it was also affected by the chemical trigger. "We see other effects as well from TERT activation, and we're working on those tissues right now," Artandi said.
Telomerase consists of the protein TERT and an RNA component, TERC. Together, they enable telomerase to perform what until now has been its only clear function: patching up chromosomes after the rigors of cell division.
Chromosomes are never completely copied during cell division but are shortened a bit at each end, where material is left out of end caps called telomeres. Eventually, when the telomeres dwindle too far down, the cell stops dividing or dies.
Though present in only modest quantities in most cells, telomerase is abundant and vital in stem cells, where ample stores of telomerase keep the telomeres nice and long, allowing the cells to keep dividing without limit.
This endless dividing of cells is fine when it's just happening in stem cells. We rely on those new cells to repair injured and worn out tissues throughout our bodies. But in 90 percent of human cancers, telomerase—normally so rare outside of stem cells—is plentiful and active, facilitating the uncontrolled growth of tumors.
"We're interested in what telomerase is doing in cancer," Sarin said. That and the hope of learning more about stem cells—as well as learning more about what TERT might be up to aside from telomere rebuilding—is what prompted the study.
To be certain it was TERT alone that was triggering the stem cells, Artandi's team crossbred mice to eliminate the presence of the RNA component, TERC. Since TERC is crucial to rebuilding telomeres, when the mice grew shaggy even with no TERC around, it was clear the follicle stem cell stimulation was due solely to TERT and that the telomere repair function of telomerase played no role.
"This is really an unanticipated effect for TERT, one that's independent of the conventional telomerase complex," Artandi said.
The findings have gotten the attention of other telomerase researchers. "It's very interesting and very tantalizing," Carol Greider, one of the co-discoverers of telomerase, was quoted as saying in an article in the New York Times on the findings. Greider is at Johns Hopkins School of Medicine and was not involved in the study.
Artandi and Sarin stressed that the potential for therapeutic treatments arising from their work is highly speculative at this stage. That caveat aside, they noted many diseases and conditions could benefit from renewed tissue, including chronic ulcers of the skin, Parkinson's disease, Type-1 diabetes, osteoarthritis and some spinal injuries. Deafness caused by the loss of hearing hair cells, the sensory cells that respond to sound, also could benefit.
Said Artandi: "It's a very long list, and it really touches on many of the principal diseases that affect people, especially with advancing age."


Share This Story