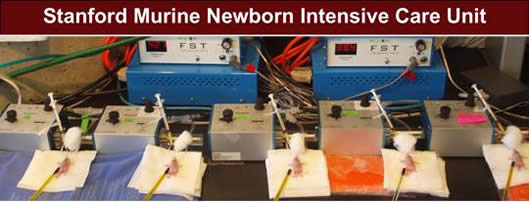
Marlene Rabinovitch, M.D. - Research Interests:
 |
Click here for detailed descriptions of ongoing research projects
Overview: Our research program seeks to identify the cellular and molecular programs regulating vascular and lung development. We then determine how these programs are perturbed by genetic abnormalities or injurious processes associated with disease. Our studies use high throughput genomic and microfluidic technologies, a variety of cell biology platforms including confocal and videomicroscopy, genetically modified mouse models of human disease, human tissue samples and induced pluripotent stem cells to answer these questions. Our major disease focus is pulmonary arterial hypertension (PAH), a condition that can be a fatal complication in children with heart defects, but also arises as a condition of unknown etiology primarily in young women. The pathological changes in the lung blood vessels that cause right-sided heart failure include loss of the distal microcirculation and obliterative proliferative changes occluding the lumen of larger arteries. Our goal is to learn how we can activate lung vascular developmental programs to regenerate lost microvessels and to reverse the obliterative changes. Over the past decade our research has led to four novel compounds in clinical trial or being positioned for clinical trial.
Our research projects have explored the link between the genetic mutation causing loss of function of bone morphogenetic protein receptor (BMPR) 2 and perturbation of Wingless (Wnt) signaling, PPARg mediated gene regulation, RNA translation, cross-talk with other cell surface receptors (PDGF, RAGE) and structural and functional derangement of the pulmonary circulation. We also address how viruses perturb microRNA function and how this might lead to the activation and production of neutrophil elastase in the vessel wall, and we use microfluidics to establish lung vascular and inflammatory cells that are transformed or abnormally expanded
New NIH funded research uses induced pluripotent stem cells in collaboration with the laboratory of Dr. Joseph Wu and next generation sequencing in collaboration with the laboratory of Dr. Michael Snyder. Our team compares endothelial cells (ECs) derived from induced pluripotent stem cells (iPSC) with native ECs, to improve our understanding of pulmonary hypertension. Towards this goal, we are comparing gene variants (by Exome/whole genome sequencing), epigenetic changes (DNA methylation, by Methyl-Seq) and RNA expression (by RNA-Seq) in iPSC-ECs derived from skin fibroblasts or blood cells,, iPSCs derived from pulmonary arterial EC, with native PAECs. from the same PAH patients or controls. Our second goal is to use iPSC-ECs derived from blood or skin of PAH patients to correct gene variants and to screen novel therapies to determine whether the EC functions of these cells normalize.
We also have an NIH Translational Program Project with the laboratories of Drs. Richard Bland and Mark Nicolls to address the vulnerable microcirculation in pulmonary hypertension, chronic lung disease of prematurity and lung transplant rejection and to work toward translation of novel therapies including the elastase inhibitor elafin. Together with the Nolan, Robinson, Utz and Kodadek Groups on an NIH Proteomics Initiative we address autoimmunity and its relationship to the development of pulmonary hypertension. We use high throughput immunophenotyping and mass element flow cytometry (CYTOF) to identify abnormalities in the immune system and in the response to viral infection.
Other investigator-initiated research focuses on the pivotal role of PPARg as a transcription factor activated by BMPR2, and its novel role in DNA damage and repair.. These studies led to investigations linking p53, with PPARg and the DNA repair machinery and others, that have uncovered a role for amphetamine-stimulated G-protein Coupled Receptor (GPCR) signaling in amplifying DNA damage.
We are engaged in creating genetically modified mice with conditional cell-specific deletion of genes, fate mapped reporter genes to trace lineage and heterozygosity to understand vascular and cardiac phenotypes. We are then positioned to use these mice to reverse disease. We address many features of altered signaling related to the BMP receptor (R2) mutated in familial forms of pulmonary hypertension. Recently we have shown that alterations in normal functioning of BMPR2 impairs elastin fiber assembly and increases susceptibility to degradation by elastase. Well-assembled elastin maintains the integrity and distensibility of vessels and prevents abnormal proliferation of underlying smooth muscle cells and fibroblasts. Abnormalities in elastin fiber assembly underlie both pulmonary arterial hypertension as well as systemic vascular diseases including aneurysm formation. Genetic studies are also investigating families with congenital heart defects and pulmonary vascular malformations or severe pulmonary hypertension.
DAPI staining of a heart–shaped lung airway (Captured by postdoctoral fellow Isabel Diebold).
Our research program harmonizes with that of Dr. Richard Bland who investigates the regulation, expression and function of genes that coordinate pulmonary alveolar and vascular development, and how they are perturbed by prematurity and mechanical ventilation, leading to chronic lung disease.
Ongoing research in the laboratory of Marlene Rabinovitch, M.D.
Richard D. Bland, M.D. - Research Interests:
Ongoing research projects
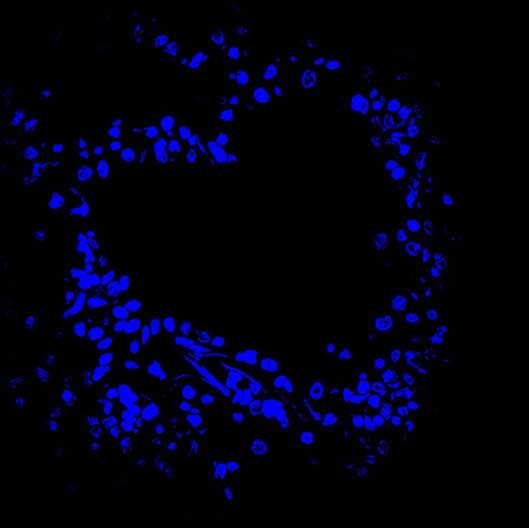
As elastin plays a crucial role in lung growth and development (elastin-null mice die soon after birth from cardiorespiratory failure related to defective alveolar and lung vascular formation), our group has a special interest in studying the effects of prolonged mechanical ventilation (cyclic lung stretch) with oxygen-rich gas (which is often needed to sustain life of extremely premature infants) on genes that regulate elastin synthesis and assembly, which in turn can affect lung septation and angiogenesis. As mechanical ventilation of developing lungs can trigger release of proteolytic enzymes that break down elastin, we recently completed studies showing that intrapulmonary treatment of newborn mice with elafin, a potent inhibitor of serine elastase activity, prevented the adverse effects of mechanical ventilation on lung growth. In addition, we recently discovered that intrapulmonary treatment of newborn mice with a neutralizing antibody to TGFß preserved VEGF signaling, prevented apoptosis and promoted lung growth during mechanical ventilation. These studies provide strong rationale for developing novel strategies to treat or prevent neonatal chronic lung disease, and perhaps other respiratory disorders that exhibit similar pathological features in older children and adults.
Ongoing research in the laboratory of Richard Bland, M.D.