Basic Science Research
 Development of a mouse model for pulmonary hypertension. More Development of a mouse model for pulmonary hypertension. More |
To lead the search toward improved understanding of the biology of pulmonary vascular disease and the discovery of new treatment modalities, Wall Center researchers are collaborating with researchers in other disciplines within the Stanford School of Medicine as well as with those at outside institutions. The recruitment of Marlene Rabinovitch, MD as the Dwight and Vera Dunlevie Professor of Pediatric Cardiology and the Director of Research for the Wall Center was a significant accomplishment and adds significant depth to the Wall Center bench and translational research programs. Dr. Rabiovitch brings with her a mature program of research into the molecular mechanisms of cardiopulmonary disorders in children. Her current research focuses on the elucidation of the cellular molecular mechanisms of vascular disease and attempt to bridge the gap between pulmonary and systemic vascular pathobiology leading to severe pulmonary vascular disease. Dr. Rabinovitch's research lab.
Basic science research in the area of pulmonary hypertension and pulmonary vascular disease is also currently being performed by Dr. Peter Kao and Dr. John Faul in the Division of Pulmonary and Critical Care Medicine, along with Dr. Ron Pearl in the Department of Anesthesia. The group has created an animal model of pulmonary hypertension, and has examined the role of nitric oxide in the treatment of pulmonary hypertension. Both of these areas of study have resulted in multiple publications.
Simvastatin attenuates smooth muscle neointimal proliferation and pulmonary hypertension in rats.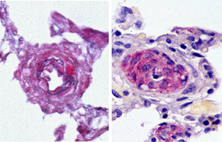 Left image: Image of diseased pulmonary artery that has been "opened up" with the use of the drug Simvastatin Right image: Image of occluded pulmonary artery from a rat with fatal pulmonary hypertension. Full article Related article |
Under the direction of Dr. Faul, the group is also investigating factors that control abnormal pulmonary arterial smooth muscle cell proliferation in patients with pulmonary vascular disease. In particular, the development and progression of pulmonary arterial neointimal formation. Since abnormal accumulation of pulmonary arterial neointimal cells leads to increased pulmonary vascular resistance and heart failure, it is a logical strategy to determine which biologic factor is required for its progression, since this knowledge would greatly enhance our search for a cure. The group is also conducting a randomized, double blind placebo-controlled study of simvastatin(Zocor) in patients with pulmonary arterial hypertension and have already demonstrated that simvastatin attenuates and even reverses established pulmonary arterial hypertension in rats through pulmonary arterial smooth muscle cell apoptosis and restoration of endothelial nitric oxide synthase activity. The long-term goal of these studies is to discover therapies with anti-proliferative effects that reverse the underlying disease, rather than medications that temporarily relieve symptoms.
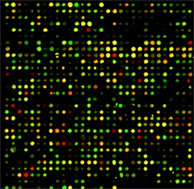
Another example of cross disciplinary efforts includes work in collaboration with the Division of Endocrinology studying autoimmune thyroid disease in PH patients. Preliminary studies have been completed and have been published. Building on this important research, a future study of auto-antibody profiling in PH patients with thyroid disease is underway with Dr. P. J. Utz in the Division of Immunology.
One of the hopes of the Wall Center is to develop alternatives to transplantation in patients with pulmonary vascular disease. In the interim, since patients with pulmonary vascular disease will continue to require transplantation, research in this area will be a focus. Stanford already has several active research programs in transplantation medicine in which pulmonary vascular biology plays a key role. Mechanisms of reperfusion injury following lung transplantation, a problem which limits transplant success and for which there is no good treatment, have been studied in collaboration with the laboratory of Dr. Robert Robbins in Cardiothoracic Surgery. Dr. Ramona Doyle has collaborated with colleagues in Liver Transplantation and Renal Transplantation at Stanford in developing a better understanding of gene expression in acutely and chronically rejecting organs.

